Removal of the uterus
This is a surgical operation that is performed to treat various gynecological diseases when other methods have proved ineffective or impractical.
Removal of the uterus (hysterectomy) is one of the most frequently performed operations in gynecology. It can be indicated for fast-growing fibroids, multiple fibroids, endometriosis, profuse uterine bleeding, malignant neoplasms of the uterus.
There are three types of hysterectomy. With radical hysterectomy, the uterus, cervix, ovaries, fallopian tubes, regional lymph nodes and surrounding fatty tissue are completely removed. With a total hysterectomy, the entire uterus, along with the cervix and appendages, is removed. And with subtotal hysterectomy, the uterine body is removed while preserving the cervix.
For hysterectomy, the following are used: Surgical instruments for incisions and tissue removal. Laparoscopic systems for minimally invasive procedures.
An examination should be performed before a hysterectomy: Consultation with a gynecologist and a surgeon. Ultrasound of the pelvic organs, if necessary — MRI or CT scan. Blood tests, including a general analysis, coagulogram and infection tests. Ultrasound of the ovaries with a Doppler to assess blood supply.
Hysterectomy can be performed using three main methods: abdominal, vaginal, or laparoscopic. Abdominal hysterectomy is performed through an incision in the lower abdomen and provides the surgeon with full access to the pelvic organs, which allows you to remove the uterus and, if necessary, other affected tissues. Vaginal hysterectomy is performed through an incision in the vagina and is suitable if there is no need for extensive surgical access. This method is less invasive. Laparoscopic hysterectomy is performed through small incisions in the abdomen using a camera and special tools. This is a minimally invasive procedure that reduces recovery time.
Recovery after hysterectomy depends on the type of surgery performed and may take different time. In laparoscopic operations, patients can get up on the same day, and discharge usually occurs 1-3 days after the intervention. After vaginal operations, activation from bed begins on the first day, and discharge – on 3-5 days. In operations with an incision in the abdomen, activation occurs on 1-2 days, and discharge occurs on 5-7 days after surgery. The general rehabilitation period after uterine extirpation takes about 1 month on average, while sexual intercourse is not recommended during the first 2 months. These figures are average and indicative, therefore, individual recommendations are given to each patient depending on age, type of surgery performed, course of the early postoperative period, concomitant diseases and other factors.
Benefits
Effective treatment
The procedures eliminate the symptoms and prevent the progression of diseases.
Different access methods
The ability to choose the most appropriate method depending on the clinical situation.
Reducing the risk of recurrence
Radical removal of the affected tissues reduces the likelihood of recurrence.
Security and predictability
Modern techniques ensure a high level of safety and predictability of the outcome.
Frequently Asked Questions
Which hysterectomy method should I choose?
How long does it take to recover from surgery?
Is it possible to exercise after a hysterectomy?
Didn't find an answer to your question?
You can describe your problem in detail and ask a question to the doctor. He will answer you and help you find a solution
Specialists
Find a SpecialistDoctor of the highest category, surgical obstetrician-gynaecologist specialising in anti-age and bioregenerative medicine, oncologist
Similar referral activities
Removal of tumors in the intimate area
A procedure aimed at eliminating benign growths such as papillomas, warts, cysts and genital warts.
Reproductive surgery
Surgical treatment and simultaneous accurate diagnosis of female infertility factors: adhesions, endometriosis, congenital malformations of the genital organs, obstruction of the fallopian tubes, intrauterine pathology (septum and synechia), polycystic ovary syndrome.
Colposcopy procedure
A procedure in which a doctor can use a colposcope to examine the vagina, cervix and vulva, examine the mucous membrane in detail and identify abnormal changes that may be a sign of diseases.
Cervical plastic surgery
Cervical plastic surgery (tracheloplasty) is a surgical restoration of the anatomical structure and function of the cervix, which helps to maintain the health of the reproductive system.
Treatment of vulvar diseases
Vulvar diseases, including chronic fissures, sclerotrophic lichen and other dermatological conditions. We offer modern and effective treatment methods aimed at reducing symptoms and restoring the normal condition of the vulva skin.
Correction of menopause problems
The onset of menopause is often accompanied by a number of physical and mental manifestations unpleasant for a woman. The gynecologist will choose therapy, which can relieve or completely eliminate the symptoms.
News & Media
All news and mediaThe III All-Russian Progress Conference "Aesthetic Gynecology and Perineology: balance of beauty and functionality" was held in Moscow
The event lasted from 24 to 26 May, and the theme was Aesthetic gynecology and perineology: the balance of beauty and functionality.
What to do with urinary incontinence after childbirth?
Find answers to your questions and feel more confident.
What is important for every woman to know about the cervix?
Everything you need to know about the cervix is now collected in one article on the website of the "Daughter-mother".
Why should your mother visit a gynecologist?
We all understand why girls should visit a gynecologist. This specialist will help solve various problems related to women's health — from pregnancy management to the prevention of sexually transmitted diseases. However, over time, when women get out of reproductive age, they begin to contact a gynecologist less and less often, mistakenly believing that they no longer need his help. But a gynecologist is not only about reproductive health, he can help in solving many other issues related to the female body. So what questions can your mother ask a gynecologist about?
How to strengthen the pelvic floor muscles?
Intimate problems are often hushed up, it is awkward to talk about them even with a doctor. However, if the issue concerns the health of the pelvic floor, it is better not to waste time and immediately consult a doctor. After all, problems with this area can lead to very unpleasant consequences.
Uterine bleeding — is it worth sounding the alarm?
Abnormal uterine bleeding is when the bleeding goes beyond the normal menstrual cycle. The discharge may be more abundant or last longer. The "normal" menstrual cycle is different for everyone. But menstruation shouldn't be a problem for you.: a serious condition that prevents you from engaging in any activity, forces you to skip work or study. In the article we will tell you how to distinguish abnormal uterine bleeding.
Stress-free menopause: how hormone therapy helps women
With age, women experience a natural decrease in reproductive function, known as menopause. This process takes a long time and is accompanied by changes in the physical and emotional state, hormonal restructuring and complete cessation of menstruation. On average, menopause (the so-called last menstruation in a woman's life) occurs at the age of 45-55 years, but its precursors may appear earlier, and the process of "restructuring" the body can last for several years. A decrease in the level of female sex hormones leads to unpleasant symptoms that not only worsen the quality of life, but can also contribute to the development of serious diseases. Although menopause is not a disease and does not require treatment, there are methods to improve well-being and prevent complications. One of these methods is menopausal hormone therapy (MGT). The decision on the need and time of MGT is made by a gynecologist. To understand whether such therapy is necessary for all women, it is important to understand the nature and characteristics of menopause.
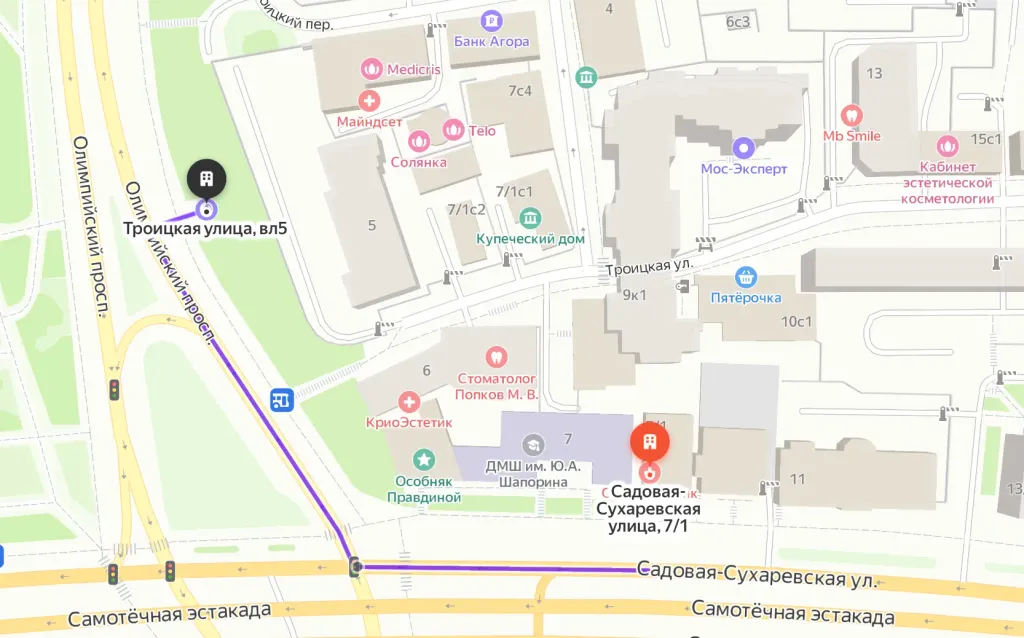
How to reach
How to get
From the Belorusskaya metro station of the Zamoskvoretskaya line - exit 4 After exiting the subway, walk through the pedestrian tunnel and climb the stairs. Move towards the railway tracks, go down the stairs immediately after them and walk along the house, then turn right onto 1st Yamskoye Pole Street. At the turn to 3rd Yamsky Pole Street, cross the road at the pedestrian crossing and continue along 1st Yamsky Field Street, after a few buildings on the left you will see Olympus Clinic MARS.
Travel time
9 minutes
Landmark
Olympus Clinic MARS sign
How to get
From the Belorusskaya metro station of the Ring line - exit 2. After exiting the subway, turn left and walk to the pedestrian crossing. Cross the road through two pedestrian crossings and move along the Tverskoy overpass. Go down the stairs immediately after the railway tracks, walk along the house, then turn right onto 1st Yamskoye Pole Street. At the turn to 3rd Yamsky Pole Street, cross the road at the pedestrian crossing and continue along 1st Yamsky Field Street, after a few buildings on the left you will see Olympus Clinic MARS
Travel time
11 minutes
Landmark
Olympus Clinic MARS sign
From the metro station "Tsvetnoy Bulvar"
1 exit to the city, then left to the Garden Ring, at the crossing to the right, crossing the boulevard, one more crossing and at the traffic light to the left. The Olymp Clinic building is located overlooking the Garden Ring to the right of the crossing. Travel time is approximately 9 minutes. Landmark - sign Olymp Clini
From the metro station "Sukharevskaya"
Exit 3 from the metro and 640 meters straight ahead, the clinic will be on the right. Landmark - sign Olymp Clinic
Parking lot map
Exit 3 from the metro and 640 meters straight ahead, the clinic will be on the right. Landmark - sign Olymp Clinic
From Sokol metro station
The last car from the center: follow the signs for Exit 5. From the glass doors to the right and go to the end of the passage. Exit to the city by the steps to the left. After exiting the crossing to the street, go straight along Leningradsky Prospekt to the intersection with Chapaevsky Lane. Next, turn right (onto Chapaevsky Lane) and walk to the Triumph Palace residential complex. Entrance to the territory: through checkpoint No. 1, opposite the Vkusville store, you will need to present your passport. After passing through the checkpoint, go up the stairs to the fountain, opposite it you will see our clinic.
Travel time
10-12 minutes
From the Airport metro station
The first car from the center: follow the Exit 2-3 signs. Turn left out of the glass doors and walk to the end of the passage. After exiting the crossing to the street, go straight along Leningradsky Prospekt to the intersection with Chapaevsky Lane. Next, turn left (onto Chapaevsky Lane) and walk to the Triumph Palace residential complex. Entrance to the territory: through checkpoint No. 1, opposite the Vkusville store, you will need to present your passport. After passing through the checkpoint, go up the stairs to the fountain, opposite it you will see our clinic.
Travel time
12-15 minutes
How to get
Entry to the territory is prohibited, but there are free city parking lots around the Triumph Palace residential complex, where you can easily find a place for your car. Free parking area:






