Endoscopic discectomy
Endoscopic discectomy is a minimally invasive surgical procedure aimed at removing pathological disc protrusion that puts pressure on the nerve, with minimal impact on the surrounding tissue.
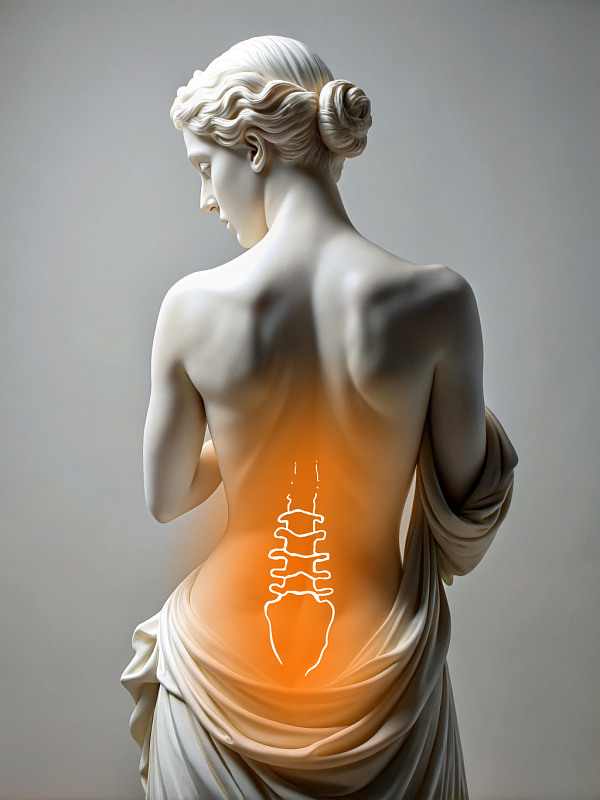
This procedure effectively relieves nerve root compression, eliminates pain, restores mobility, and prevents neurological complications. This technique is used for hernias in the lumbar, thoracic, and cervical spinal regions, and it is recommended when nonsurgical treatment has been unsuccessful. The procedure can be performed regardless of complexity, depending on the size and location of the hernia and the patient's condition.
Before the operation, the patient must undergo a standard set of tests. These include a complete blood count and biochemical analysis, infection tests, an ECG, a spinal MRI, and necessary specialist consultations. Ten hours before the procedure, the patient should refrain from eating or drinking anything, including water. In some cases, hospitalization the day before is recommended. Preparation also includes informing the patient about the postoperative period.
The patient is positioned on the operating table. After administering general anesthesia, the surgeon makes a 7 mm incision in the skin and inserts an endoscope through it. The surgeon then guides the endoscope to the affected intervertebral disc using X-ray guidance. Then, a microinstrument is inserted through the endoscope channel to the hernia. This instrument is used to remove the protrusion in stages under visual control. A high-definition camera transmits an image to a monitor, enabling the surgeon to perform precise manipulations in a confined space. Only the pathological area of the disc is removed, not the entire disc. Once the procedure is finished, the incision is closed with an intradermal cosmetic suture that does not require removal, and a bandage is applied.
Endoscopic surgery involves using a high-precision, advanced system that includes a thin endoscope with a 4K camera, microinstruments, and an X-ray machine for navigation.
Patients can walk within two hours after surgery and may be discharged on the day of or the day after surgery. For the first few weeks, it is recommended that the patient wear a corset or orthopedic collar (depending on the area of intervention), limit physical activity, and take a course of medication. Later on, the patient is advised to undergo exercise and physical therapy to strengthen their muscles and restore segmental stability. They should avoid heavy lifting and carrying heavy objects for a month. A follow-up appointment is scheduled 30 days later.
Benefits
Minimal trauma
The surrounding tissues are virtually unaffected.
Quick recovery
The patient may return home on the day of or the day after the operation
Precision
A magnifying camera displays small anatomical structures
Comfort
No large incisions are required and no spinal fixation is performed
Врачи
Смотреть всех врачейOrthopedic Trauma Surgeon, Vertebrologist
General surgeon, Professor, Doctor of Medical Sciences. Head of the Spine Surgery Department.
Similar referral activities
Endoscopic stenosis decompression
Endoscopic stenosis decompression is a minimally invasive surgical procedure designed to relieve pressure on the spinal cord and nerve roots caused by narrowing of the spinal canal.
Scoliosis and kyphosis spine surgery (Spine straightening)
Surgical treatment for scoliosis and kyphosis is performed when the spinal curvature progresses and causes pain or impaired posture, or when the patient has a pronounced cosmetic defect. The procedure aims to restore the correct spinal alignment, address cosmetic deformities, and stabilize the spine.
X-ray-guided transforaminal injection (1 zone)
X-ray-guided transforaminal injection provides targeted relief for pain caused by pinched or inflamed nerve roots in the intervertebral foramen area. This method ensures the accurate administration of drugs with minimal trauma.
Goel-Harms fixation
Goel-Harms fixation is a standard decompression and stabilization technique used for compression fractures, spinal stenosis, segmental instability, or spondylolisthesis.
X-ray-guided facet joint injection (1 spinal segment)
X-ray-guided facet joint injection is a minimally invasive procedure aimed at eliminating pain caused by inflammation or degenerative-dystrophic changes in the facet joints of the spine.
X-ray-guided knee or hip joint nerve injection
Knee or hip joint nerve block is an injection procedure that helps relieve pain caused by degenerative, inflammatory, or postoperative changes in the joints.

